
I chose home-based care for a reason … for the colour, the smells, the unique vibe of each family and home. I can connect with “James” and his family but I have a vague relationship with “the guy with bladder cancer.” James with the porcelain dolls standing as sentinels on the shelf is a unique person, in a unique environment, with a unique family care team. The guy with bladder cancer … instead of James with the dolls. Now, my patients have been reduced to their diagnosis. It is like caring for “person A in bed B” instead of James with the porcelain dolls displayed behind him. It is closer to the limitations of institutional care than it is to quality home-based care. “Which doctor are you again? Why has this visit been scheduled?” they might ask.Ĭaring for people virtually at home is limiting. I no longer feel I know my patients because my lens has narrowed my senses are limited and I’m caring for people through tunnel vision.Īnd I am convinced that the patients and families feel the same way about me. Once or twice, I have even wondered if I was experiencing early dementia. I’ve lost a part of my patients … and their families. In the following weeks, someone will say to me, “You remember James, don’t you? The man in the dining room with the porcelain dolls watching over him?” Boom, James is in perfect view in my mind.īut not now. Later, as I sit down to document, the patients’ story will replay in my mind and the details remain vivid. I never take notes while I’m in the home. When I leave, I can taste the rancid air in my mouth and it lingers in my hair until I write my consult note that evening. The room is heavy with the smell of cigarette smoke and kitty litter. The dolls make me feel like I’m being watched. The porcelain doll collection is standing guard in the cabinet. Their home is more disorganized and there are dishes piled high in the sink.

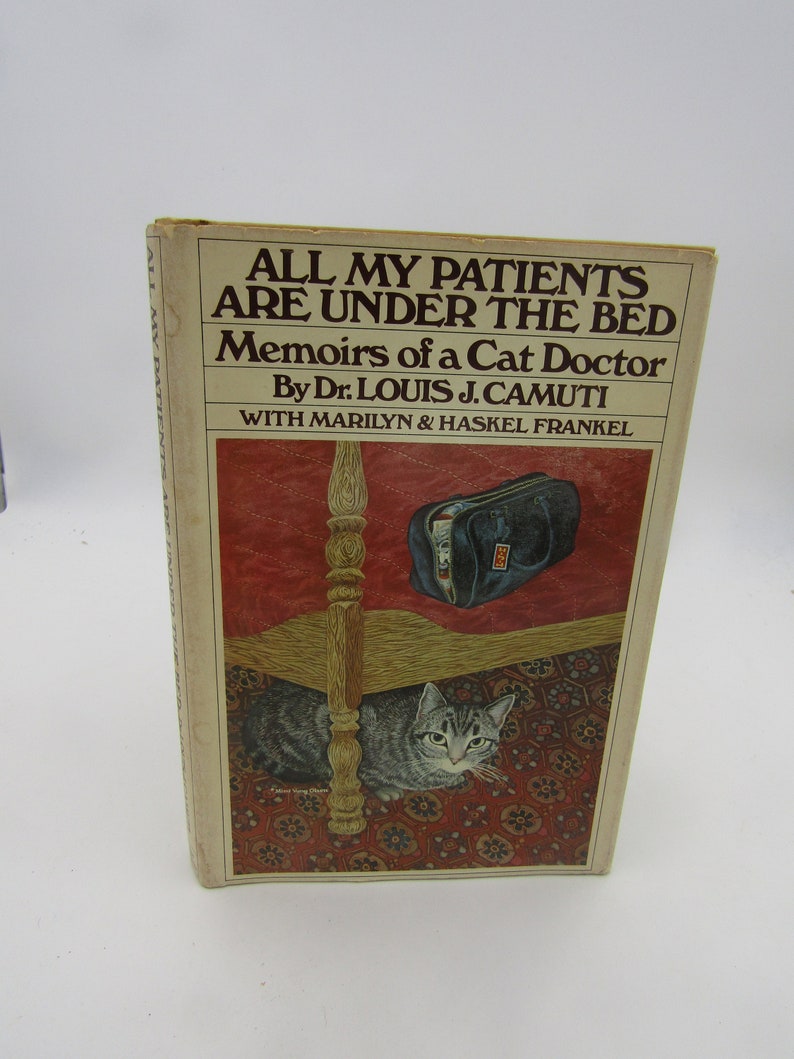
Our patient is lying in a hospital bed in the makeshift bedroom that was the dining room last week. She’s not usually dressed in her PJs at 2 p.m., we realize. Jones, the caregiver to her husband, James, is very unkempt compared to her baseline tidiness. This intel gathering continues as we notice how long it takes for the door to be answered, who comes to the door, what they are wearing and the state of their readiness for the visit.įor example, Mrs. The state of the home and the caregiver is often a clue to a patient’s wellness and provides insights to what is happening inside the home. This starts from the time we drive up to the home, notice the state of the grounds, the type of garbage in the bins, the unshovelled snow on the unsalted driveway or unwatered flowers wilting in garden pots. We home-care clinicians use all of our senses when we meet patients and their families while doing an assessment. Home-based care requires a skill set that isn’t taught in medical training. Because now, more than ever, I am convinced that home-based medical care is critically unique from all other types of care delivery. It’s taken the entire year of the pandemic for me to figure out what the problem was. “These are crazy times” was another way of explaining any shift from normal. So, what was happening? Why couldn’t I remember my patients anymore? What brought this tedium upon me? I chalked everything up to “the pandemic,” even though I wasn’t quite sure how my dissatisfaction was the result of the changes made in my practice. “Yes, of course I remember her,” I would say. It used to be that a team member would mention a patient’s name followed by, “You know, the woman with all the cats,” or “The man with the artwork covering his walls.” Immediately, I would remember the patients their faces would come into focus and their overarching illness story would replay in my mind. Their faces were blurred and I couldn’t recall any physical images of them by name or address. But it didn’t take long for me to realize something was missing.įor the first months of virtual home visits, I thought the stress of the pandemic might be affecting my memory because, unlike previously, I was losing important elements of my patients and their surroundings between consults. At first, I thought virtual care would revolutionize my practice after all, it would minimize driving time and maximize the number of patients I could care for in a day. I have always struggled with technology, so I had to learn the bare minimum to continue to look after my patients.

When the pandemic hit, like many of my colleagues, I converted my practice to virtual-based care. I’ve been caring for people in their homes for 15 years as a palliative care physician.


 0 kommentar(er)
0 kommentar(er)
